PART 3: LEAN SIX SIGMA ACROSS INDUSTRIES
12 Chapter 12: Lean Six Sigma in Healthcare
Learning Objectives
- Analyze how Lean Six Sigma can improve patient flow and reduce wait times.
- Devise strategies for eliminating medical errors and enhancing safety.
- Evaluate Lean Six Sigma as applied in hospital operations for operational excellence.
Learning Outcome:
Describe the implementation process for Lean Six Sigma in a Healthcare environment.
Introduction
Lean Six Sigma combines Lean principles, which focus on waste reduction, with those of Six Sigma, which emphasize reducing variation and improving quality. When applied to healthcare, Lean Six Sigma can bring about significant improvements in patient care, operational efficiency, and overall hospital performance.
Some common examples of LSS’s many applications are detailed in this chapter.
Improving Patient Flow and Reducing Wait Times
Understanding Patient Flow
Efficient patient flow ensures that patients receive timely care, reducing overcrowding and improving overall satisfaction. In a healthcare environment, this involves the smooth transition of patients through various stages, through various stages. For example, from admission to discharge (inpatient), check in to check out (ambulatory), and arrival to admission (ED) See cases at the end of this chapter.
Identifying Bottlenecks
Lean Six Sigma tools, such as value stream mapping (VSM) and process mapping, are instrumental in identifying bottlenecks in patient flow. These tools provide a visual representation of the entire patient’s journey, highlighting areas where delays and inefficiencies occur.
5S Methodology
Organizing and standardizing the work environment with the 5S methodology (Sort, Set in order, Shine, Standardize, Sustain) reduces unnecessary inventory as well as the time that staff spend searching for equipment and supplies, and thus speeds up patient care.
Kanban Systems
Implementing a Kanban card system for inventory management ensures that necessary medical supplies are always kept at an ideal stock level – neither running out nor overstocked reducing delays in treatment. This is different from the card used on a Kanban Board to track progress. (See Just-In-Time)
Scheduling Optimization
Using Six Sigma’s DMAIC (Define, Measure, Analyze, Improve, Control) approach, hospitals may analyze patient arrival patterns and optimize scheduling to reduce wait times.
Case Study: A community hospital implemented Lean Six Sigma to improve its emergency department (ED) patient flow. By mapping the patient’s journey and identifying key bottlenecks, the hospital reduced average wait times, from 90 to 45 minutes, within six months.
Eliminating Medical Errors and Enhancing Safety
Root Cause Analysis
Lean Six Sigma employs Root Cause Analysis (RCA), using techniques such as fishbone diagrams and the Five Whys to identify the underlying causes of medical errors.
Error Proofing
Poka-yoke: This Lean technique involves creating fail-safes to prevent errors. For instance, color-coding medications and implementing barcoding systems can reduce errors in administering medications.
Standard Work: Developing standardized procedures for common tasks ensures consistency and reduces the likelihood of errors.
Improving Communication: Using the SBAR (Situation, Background, Assessment, Recommendation) communication framework improves information exchange among healthcare providers, reducing misunderstandings and errors.
Case Study: A major hospital reduced medication errors by 40% after implementing a Lean Six Sigma project to standardize medication administration processes and enhance staff training.
Leveraging Lean Six Sigma in Hospital Operations
Operational Efficiency
Lean Six Sigma can streamline various hospital operations, including admissions, discharge processes, and laboratory services.
Lean Tools
Kaizen: Regularly scheduled Kaizen huddles and events encourage continuous improvement, as they involve staff in identifying and implementing small, incremental changes.
Gemba Walks: Leaders conduct regular Gemba walks to observe work processes firsthand, understand challenges, and gather ideas for improvement, as well as feedback and ideas from frontline staff and managers.
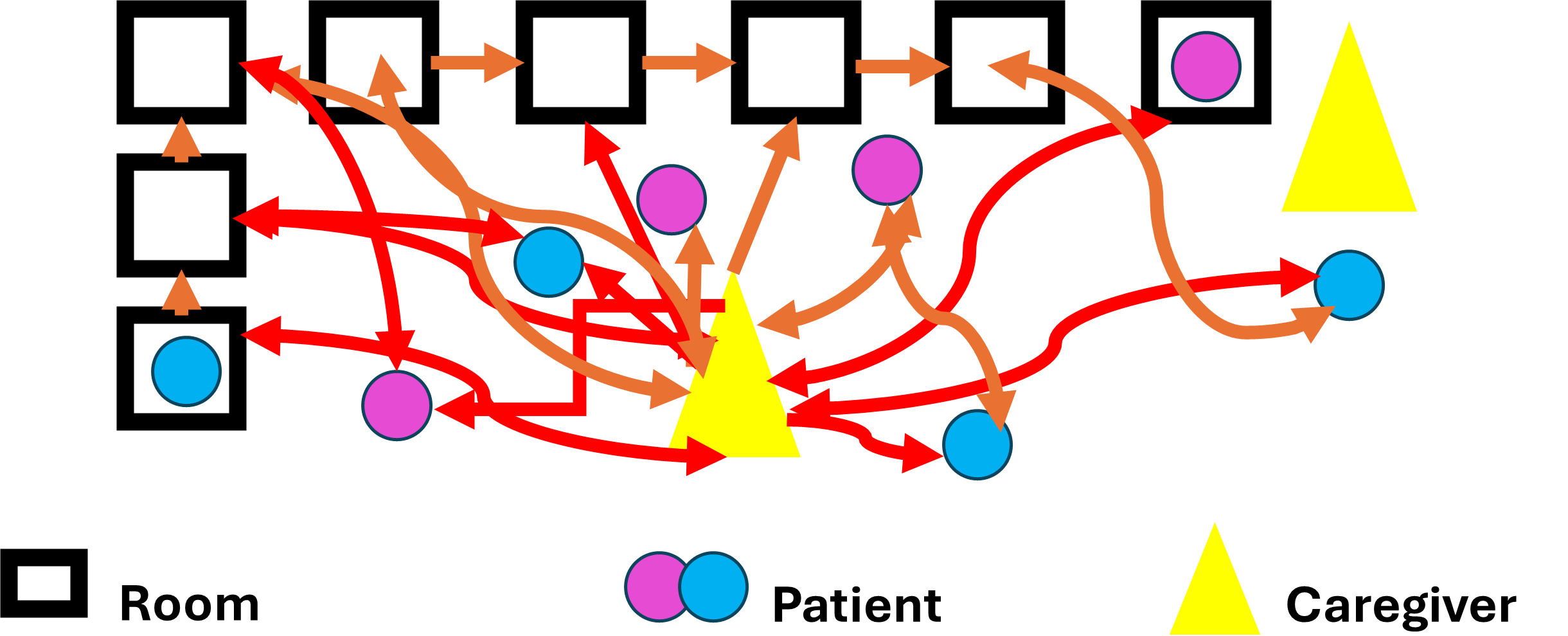
Spaghetti Diagrams: A spaghetti diagram visually represents the flow of materials, information, or people within a process. It uses continuous lines to identify inefficiencies, redundancies, and unnecessary movements in order to enhance workflow and optimize layout.
Six Sigma Tools
Control Charts: Monitoring key performance indicators (KPIs) with control charts helps to monitor/track and maintain process improvements and identify when processes deviate from standards.
Pareto Analysis: Focusing on the most critical issues, as identified by Pareto analysis, ensures that resources are directed toward solving the most impactful problems.
Case Study: A regional medical center implemented Lean Six Sigma to optimize its discharge process. This reduced the average discharge time by 30% and freed up beds more quickly for incoming patients.
Achieving Operational Excellence in Healthcare
Key Performance Indicators (KPIs)
Tracking and analyzing KPIs such as patient satisfaction, readmission rates, and the average length of stay provide insights into hospital performance and illuminates areas for improvement, e.g., wait times, productivity, scheduling lab/delays, and so on.
Scheduling Optimization
Using Six Sigma’s DMAIC (Define, Measure, Analyze, Improve, Control) approach, hospitals can analyze patient arrival patterns and optimize the staff schedule to reduce patient wait times. For instance, by studying the peak times for patient arrivals, a hospital can allocate more staff during these periods to reduce bottlenecks. A study by Litvak et al. (2005) demonstrated that optimizing schedules based on patient flow data reduced wait times by 25% in an emergency department.
Error Proofing
Implementing fail-safe, or Poka-yoke, is essential in reducing medical errors. For example, the use of barcode scanning for medication administration ensures that the correct medication is given to the correct patient at the correct dose and time. A study by Poon et al. (2010) found that barcode-assisted medication administration reduced errors by 41.4%.
Cultural Change
Achieving operational excellence requires an organizational culture shift towards continuous improvement. Engaging all staff, from frontline workers to executives, is crucial for fostering a culture that supports Lean Six Sigma principles.
Leadership Commitment
Leaders must champion Lean Six Sigma initiatives by modeling commitment through their actions and communications. Leadership should actively participate in improvement projects, allocate resources, and recognize contributions. A strong leadership presence can drive the organizational culture towards embracing change and prioritizing quality improvements.
Employee Involvement
Engaging employees is essential to creating a culture of continuous improvement. This can be achieved by:
Training and Development: Ongoing Lean Six Sigma training helps staff understand its methodologies and their benefits, and it enables them to contribute effectively to improvement efforts.
Idea Generation: Encouraging staff to submit ideas and engage in generating solutions for change management and process improvements fosters a sense of ownership and empowers staff to take part in shaping their work environment. Tools such as suggestion boxes or regular brainstorming sessions may facilitate generating and collecting ideas.
Recognition and Rewards: Acknowledging and rewarding employees for their contributions to improvement projects reinforces positive behavior and motivates others to participate.
Communication: Effective communication is key to maintaining a culture of continuous improvement. Regular updates on project progress, successes, and challenges keep everyone informed and aligned with the organization’s goals. Transparent communication helps build trust and ensures that all staff understand how their efforts contribute to the overall objectives.
Sustainability: To sustain a culture of continuous improvement, it is important to take the following steps:
- Embed Lean Six Sigma into Daily Practices: Make Lean Six Sigma principles a part of everyday activities. Integrate them into standard operating procedures and performance evaluations.
- Conduct Regular Reviews: Periodic reviews of processes and outcomes ensure that employees maintain improvements and adapt them as necessary. Setting up review committees or working groups that regularly assess progress and make adjustments is essential.
- Promote a Growth Mindset: Encourage employees to maintain a growth mindset in which challenges are seen as opportunities for learning and improvement, rather than setbacks. This mindset helps to overcome resistance to change and promotes resilience within the organization.
Case Study: A large healthcare system successfully embedded Lean Six Sigma into its organizational culture, resulting in a 20% improvement in patient satisfaction scores and a significant reduction in operational costs. By investing in comprehensive training, actively involving employees in improvement projects, and maintaining open lines of communication, the organization created a robust culture of continuous improvement that resulted in long-term operational excellence.
Cleveland Clinic: A Case Study of a TPS-Inspired Approach to Healthcare
Cleveland Clinic, a world-renowned healthcare institution, implemented a tiered huddle system in 2018. The organization used the Toyota Production System’s (TPS) emphasis on continuous improvement and efficient communication for its inspiration. These tiered huddles consist of brief, focused conversations that occur daily across the hospital. They cover key topics like KPIs, operational barriers, ideas for improvement, and more, and they create a direct line of communication from frontline staff to executive leadership.
Structure and Process: The tiered huddle system at Cleveland Clinic operates as follows:
- Tier 1: Unit-level huddles (frontline staff and immediate supervisors)
- Tier 2: Department-level huddles (managers and directors)
- Tier 3: Hospital-level huddles (senior leadership)
Each tier escalates critical issues that cannot be resolved at lower levels, ensuring that problems are addressed promptly and efficiently.
Benefits to Operations:
- Rapid Problem-solving: Issues identified at the bedside can be escalated and often resolved within 24 hours. This mirrors the TPS emphasis on immediate problem solving.
- Improved Communication: The daily huddles create a structured forum for sharing information across all levels of the organization, which enhances overall communication and transparency.
- Empowered Frontline Staff: Caregivers at all levels feel heard, and thus empowered to contribute to problem-solving, aligning with the TPS principle of respect for people.
- Enhanced Patient Safety: The “laser focus on safety” mentioned by Sue Collier, DNP, RN, NEABC, ensures that potential safety issues are quickly identified and addressed.
- Standardized Approach: The consistent structure of the huddles across all departments, hospitals, sites, and clinics reflects standardization, a key TPS principle.
Benefits to Executive Management:
- Real-time Insights: Executives gain daily, direct insights into frontline operations, allowing them to make more informed decisions.
- Efficient Resource Allocation: By quickly identifying systemic issues, leadership can allocate resources more effectively to address the root causes.
- Culture of Continuous Improvement: The huddle system fosters a culture of ongoing improvement and problem solving throughout the organization.
- Leadership Development: As noted by Shannon Pengel, MSN, RN, NEBC, the huddles provide opportunities for leaders to model and develop delegation and problem-solving skills.
- Alignment with Organizational Goals: The tiered structure ensures that KPIs are regularly reviewed at all levels and that issues are prioritized according to the organization’s strategic objectives.
The implementation of tiered huddles at Cleveland Clinic demonstrates how TPS principles can be effectively adapted to healthcare settings. By creating a structured system for rapid communication and problem-solving, Cleveland Clinic has enhanced its operational efficiency and empowered all levels of its staff. This approach not only improves patient care but also provides executive management with valuable insights for strategic decision-making. This program embodies the TPS principles of continuous improvement and respect for people.
Below are two common healthcare situations in which Lean Six Sigma can improve patient satisfaction.
1. Outpatient Situation: Reducing Appointment Waiting Times
Problem: Long wait times for patients in outpatient clinics are a common issue. They lead to patient dissatisfaction and potential loss of revenue. Inefficient scheduling, variability in patient arrival times, and service delays contribute to this problem.
Applying Lean Six Sigma Approach:
- Define: Identify the problem clearly, i.e., patients wait an average of 30 minutes past their scheduled appointment times.
- Measure: Collect data on the duration of each appointment, patient arrival time, and how long each waits before seeing a doctor.
- Analyze: Use tools like Pareto charts and fishbone diagrams to identify root causes, such as overbooking, inconsistent appointment lengths, or bottlenecks in the check-in procedures.
- Improve: Implement changes such as standardizing check-in procedures, optimizing the schedule based on average appointment lengths, and using reminders to reduce no-show rates.
- Control: Monitor wait times continuously with tools like control charts to ensure the improvements are maintained and adjust the schedule as needed.
Outcome: Reduced patient wait times, increased patient satisfaction, and improved clinic efficiency.
2. Emergency Department (ED): Streamlining Patient Triage Process
Problem: Emergency departments often face overcrowding and long waiting periods for non-critical patients. This can delay treatment for those who need it most and increase stress for ED staff.
Lean Six Sigma Approach:
- Define: The problem is identified as delays in patient care due to an inefficient triage process.
- Measure: Data collection focuses on time stamps for key points in the triage process: arrival, triage assessment, and initial treatment.
- Analyze: Use tools like value stream mapping to identify non-value-added steps in the triage process. Look for delays caused by unnecessary paperwork, unclear protocols, or inconsistent prioritization.
- Improve: Implement a fast-track system for minor injuries, standardize triage protocols to reduce variation, and assign clear roles for staff to handle the various triage levels.
- Control: Use metrics like patient flow rates, triage accuracy, and average waiting time to ensure consistent application of new processes.
Outcome: Shortened wait times for all patients, reduced overcrowding, and more efficient allocation of staff resources. This leads to better quality care in critical situations.
These examples illustrate how Lean Six Sigma methodologies – reducing waste, standardizing processes, and continuously monitoring results – can significantly improve healthcare service delivery in diverse settings.
Chapter Summary
References:
- Ben-Tovim, D. I., Bassham, J. E., Bolch, D., Martin, M. A., Dougherty, M., & Szwarcbord, M. (2007). Lean thinking across a hospital: redesigning care at the Flinders Medical Centre. Australian Health Review: a publication of the Australian Hospital Association, 31(1), 10–15. https://doi.org/10.1071/ah070010.
- Chassin, M. R. & Loeb, J. M. (2013), High-reliability health care: Getting there from here. Milbank Quarterly, 91, 459-490. https://doi.org/10.1111/1468-0009.12023.
- Graban, M. (2016). Lean Hospitals: Improving quality, patient safety, and employee engagement, Third Edition (3rd ed.). Productivity Press. https://doi.org/10.4324/9781315380827.
- Kaplan, G. S., Patterson, S. H., Ching, J. M., & Blackmore, C. C. (2014). Why Lean doesn’t work for everyone. BMJ Quality & Safety, 23(12), 970-973.
- Poon, E. G., Keohane, C. A., Yoon, C. S., Ditmore, M., Bane, A., Featherstone, E., & Gandhi, T. K. (2010). Effect of barcode technology on the safety of medication administration. New England Journal of Medicine, 362(18), 1698-1707. https://doi.org/10.1056/NEJMsa0907115
- Tucker, A. L., & Edmondson, A. C. (2003). Why hospitals don’t learn from failures: Organizational and psychological dynamics that inhibit system change. California Management Review, 45(2), 55-72.

