Chapter 10.0: Alcohol
Ch. 10.1: The Nature and Effects of Alcohol
- “Alcohol is a toxic and psychoactive substance with dependence producing propensities” (WHO, n.d.).
- Globally, alcohol is a leading risk factor in the burden of disease, contributing to 5.3% of all deaths (an estimated 3 million deaths) in the year 2016 (Popova, Rehm, & Shield, 2020) and accounting for 10% of all premature deaths among individuals aged 15-49 years (WHO, n.d.).
- “The harmful use of alcohol is a causal factor in more than 200 disease and injury conditions” (Popova, Rehm, & Shield, 2020).
- Alcohol misuse is also associated with a collection of social problems, including intimate partner violence, sexual assault, child maltreatment, human trafficking, problem gambling, housing insecurity, sexual risk-taking and unintended pregnancy, and suicidality (Begun, Clapp, & The Alcohol Misuse Grand Challenge Collective, 2015).
Alcohol Metabolism
Alcoholic beverages, when consumed, are broken down (metabolized) by the body—much of the work being performed by enzymatic actions directed by the liver and somewhat involving kidney functions. The ethanol molecules begin to be metabolized by an enzyme called alcohol dehydrogenase (ADH) and others (Zakhari, n.d.). This first-step metabolic process results in the alcohol turning into acetaldehyde (NIAAA, 2007). Acetaldehyde is a relatively toxic substance responsible for many of the negative health effects associated with drinking alcohol: not only is it carcinogenic (https://pubs.niaaa.nih.gov/publications/aa72.htm) and contributing to liver disease, it contributes to “hangover” symptoms (nausea and headache) when alcohol is used in excess. Acetaldehyde is subsequently metabolized by another enzyme, aldehyde dehydrogenase (ALDH) (NIAAA, 2007) and eventually excreted from the body.
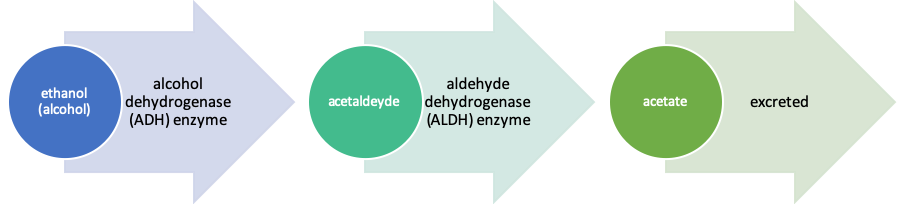
Human genetics play a significant role in directing the control and production of the metabolizing enzymes (ADH and ALDH), reflecting one mechanism in individual differences in alcohol responses. Some individuals experience a very negative (punishing) “flushing” response to consuming alcohol—a reaction sometimes considered to be protective against alcohol misuse and alcohol use disorder (AUD). This response is driven by acetaldehyde building up because the person has a deficiency in ALDH2—the enzyme is slow to break down the toxic chemical acetaldehyde. Low ALDH enzyme concentration is also associated with an increased risk of esophageal cancer among individuals who drink alcohol for much the same reason—the acetaldehyde lingers in higher concentrations before being broken down into safer, less toxic chemicals. The medication known as Antabuse works by blocking ALDH activity, allowing the build-up of acetaldehyde which leads to unpleasant side effects (including nausea/vomiting)—this “punishment” is intended to discourage someone from drinking alcohol again in the future.
Standard drink measurement. If a person indicates that they consumed one drink, do we really know how much alcohol they consumed? “One drink” could mean very different things under different circumstances.
To help address this, the U.S. National Institute on Alcohol Abuse and Alcoholism (NIAAA, 2016) published a standard drink measure protocol. This chart shows one standard drink equivalent for beer (5% ABV), wine (12% ABV), and distilled spirits/“hard liquor” (40% ABV).
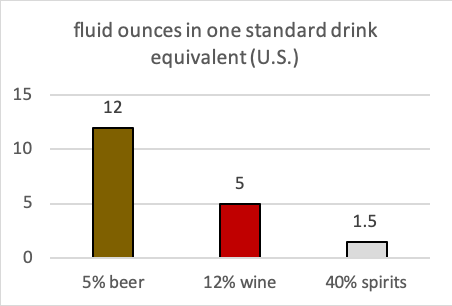
The mathematical formula for calculating standard drink equivalents is as follows:
- multiply the number of fluid ounces by the % alcohol content converted to decimal (40% being 0.40; divide % by 100 or move decimal two places to the left)
- divide that result by 0.6 ounces of pure alcohol per drink-equivalent
- the result is the standard drink equivalents involved.
For example, someone consuming a 40-ounce beer (a “forty”) of 9% ABV has consumed 6 standard drink equivalents [1 x 40 x .09 divided by 0.6]. On the other hand, a six-pack of 12 ounce “lite” beers of 4.2% ABV would be 5 standard drink equivalents [6 x 12 x .042 divided by 0.6].
Alcohol consumption guidelines and definitions. According to the 2015-2020 Dietary Guidelines for Americans published by the U.S. government (Department of Health and Human Services and Department of Agriculture), alcohol should only be consumed in moderation and only by individuals who have attained the minimum legal drinking age (currently, age 21 years across the U.S.). Traditionally, moderate drinking meant up to 1 standard drink equivalent per day for women and up to 2 drinks per day for men (https://health.gov/dietaryguidelines/2015/guidelines/appendix-9/). However, recent guidance is recommending that 1 standard drink should apply to both men and women since increased alcohol consumption is linked to increased death from all causes (https://www.dietaryguidelines.gov/sites/default/files/2020-07/PartA_ExecSum_first-print.pdf). The guidelines also acknowledge individual differences in alcohol metabolism—differences related to body mass, body composition, and metabolizing enzymes.
The recommendation is no alcohol for:
- Women who are pregnant
- Individuals under the minimum legal drinking age
- Individuals taking certain types of medication
- Individuals having certain types of health or mental health conditions
- People in recovery from an AUD, or find themselves unable to control their drinking when they do drink alcohol
Binge drinking (heavy episodic drinking) is defined as consuming 4 or more drinks within about 2 hours by women and 5 or more drinks in 2 hours by men. “Binge drinking is associated with a wide range of health and social problems, including sexually transmitted diseases, unintended pregnancy, accidental injuries, and violent crime” (Dietary Guidelines 2015-2020).
Heavy drinking is defined as 8 or more drinks per week for women and 15 or more drinks per week for men. Half of individuals engaged in 2 or more heavy drinking days per week experience a diagnosable AUD (NIAAA, 2016).
High-risk drinking is defined as 4 or more drinks on any day (binge drinking) or 8 or more drinks per week for women (heavy drinking), and 5 or more drinks on any day (binge drinking) or 15 or more drinks per week for men (heavy drinking). The “risk” refers to health concerns in general, not simply a risk for alcohol use disorder; it takes into consideration many chronic diseases and risks (e.g., violence) associated with regular binge or heavy drinking.
|
Low-Risk (Moderate) Drinking Limits (adapted from NIAAA, 2016) |
||
|
Time Frame |
Men |
Women Or Anyone Over Age 65 |
|
any single day |
no more than 4 standard drink equivalents |
no more than 3 standard drink equivalents |
|
|
AND |
AND |
|
per week |
no more than 14 standard drink equivalents |
no more than 7 standard drink equivalents |
|
Less or no alcohol may be best depending on health, medications, and how alcohol affects you; none is recommended for adolescents and pregnant women. |
||
Alcohol Effects
Alcohol is a potentially addictive substance associated with the development of tolerance and (potentially fatal) withdrawal syndrome: alcohol use disorder (AUD) is a recognized diagnosis in the DSM-5 and ICD-11. As it is a central nervous system (CNS) depressant, combining alcohol with other substances can be dangerous (especially with other CNS depressants). Furthermore, consuming alcoholic beverages:
- affects a wide range of central nervous system structures and processes,
- increases the risk for intentional and unintentional injuries
- increases the risk for adverse social consequences
- has considerable toxic effects on the digestive- and cardiovascular systems
- is classified as carcinogenic,
- “as an immunosuppressant increases the risk of communicable diseases, including tuberculosis and HIV” (WHO, n.d.).
The probability of experiencing alcohol dependence during a person’s lifetime is 4 times greater if drinking alcohol began before age 15 years (compared to individuals whose drinking is delayed until age 21 years); that probability is reduced by 14% with each increasing year of age first use of alcohol is delayed (Windle & Zucker, n.d.). Children who even sip alcohol (often with parental consent) by the 6th grade have significantly greater odds of drinking full drinks, getting drunk, and drinking heavily by the time they are in 9th grade (Jackson, Barnett, Colby, & Rogers, 2017). In other words, early sipping is not the protective factor that many parents believe it to be; “offering even just a sip of alcohol may undermine messages about the unacceptability of alcohol consumption for youth” (Jackson, Barnett, Colby, & Rogers, 2017, p. 212).
Risks associated with alcohol use increase in a dose-dependent manner, meaning that the risks increase with greater volumes of alcohol frequently consumed and increase exponentially with high volume consumption on a single occasion—binge drinking (WHO, n.d.). Not only is the amount consumed relevant, but also the rate at which it is consumed. Rate matters because the amount of alcohol circulating in a person’s system is determined by the rate at which it is metabolized and eliminated. Drinking a great deal of alcohol very quickly means that the circulating alcohol level is temporarily higher than if the same amount were to be consumed gradually over many hours—the body takes time to break down the alcohol as it is consumed.
Blood alcohol concentration (BAC). BAC refers to the percent of alcohol (ethanol) circulating in a person’s blood stream measured in parts alcohol per 1000 parts of blood. In other words, a blood alcohol concentration (BAC) of 0.10% is 1 part alcohol per 1000 parts blood (https://alcohol.stanford.edu/alcohol-drug-info/buzz-buzz/what-bac). Sometimes the term blood alcohol level (BAL) is used instead. The U.S. current national guideline used to determine when a person is unable to safely operate a motor vehicle is BAC (or BAL) or 0.08%. However, other nations set the level lower since sufficient impairment may occur at levels of 0.06% to make driving unwise and unsafe—lower BAC criteria for determining a person is under the influence (DUI) or intoxicated (DWI) are being promoted by lobbying groups in the U.S, as well. A BAC of 0.01% is indicative of alcohol consumption which is relevant to assess underage drinking.
BAC is affected by the dose/amount of alcohol consumed, the rate at which it is consumed, and person-specific factors such as body weight, biological sex, medications (and use of other legal or illicit substances), general health status, tolerance, differences in alcohol metabolizing (driven to a great extent by genetics), and to some extent whether food is also consumed. The following table (adapted from https://alcohol.stanford.edu/alcohol-drug-info/buzz-buzz/what-bac) identifies what you might expect to see in the behavior of a relatively young, healthy person whose drinking has led to different blood alcohol concentrations (BAC)—outcomes would be different in someone who routinely drinks heavily and has developed some degree of tolerance to alcohol.
|
BAC |
Likely Observed Effects |
|
0.01%-0.03% |
No obvious apparent effects; slight mood elevation |
|
0.04%-0.06% |
Sense of relaxation, warmth; minor impairment of reasoning and memory |
|
0.07%-0.09% |
Mildly impaired balance, speech, vision, and control |
|
0.10%-0.12% |
Significantly impaired motor control; poor/loss of judgment; slurred speech |
|
0.13%-0.15% |
Grossly impaired motor control; blurred vision; significant loss of balance; anxiety/restlessness |
|
0.16%-0.20% |
dysphoria (disturbed mood); nausea; “sloppy drunk” appearance |
|
0.25%-0.30% |
Severe intoxication; unable to walk unassisted; mental confusion; nausea/vomiting; dysphoria (disturbed mood) |
|
0.35%-0.40% |
Loss of consciousness; brink of coma |
|
>.40% |
Coma; likely respiratory failure leading to death |
A number of internet tools and phone apps are available for individuals to estimate their BAC. These are not guaranteed to be accurate but can provide information relevant to making decisions about continued drinking and/or driving. For example, the interactive BAC calculator at https://alcoholaddictioncenter.org/resources/bac-calculator/ uses standard drink equivalents, biological sex, body weight, and time since the first drink to compute an estimated BAC. Working a few examples varying factors results in the following estimates—the last column concerns an alarming practice whereby a person attempts to consume 21 drinks on their 21st birthday: this is potentially a lethal act (note above that BAC over 0.40% may be fatal—this is called acute alcohol poisoning). Many of the other combinations result in BACs over the legal limit (0.08%) for operating a motor vehicle.
|
male |
female |
male |
female |
male |
female |
male |
|
180 # |
180 # |
180 # |
140 # |
180 # |
140 # |
480 |
|
5 drinks |
5 drinks |
5 drinks |
5 drinks |
2 drinks |
2 drinks |
21 drinks |
|
2 hours |
2 hours |
4 hours |
4 hours |
2 hours |
2 hours |
4 |
|
BAC estimate: 0.11% |
BAC estimate: 0.14% |
BAC estimate: 0.08% |
BAC estimate: 0.15% |
BAC estimate: 0.03% |
BAC estimate: 0.05% |
BAC estimate: 0.54% |
Alcohol tolerance and withdrawal. Earlier chapters discussed the definition and biological processes of developing tolerance and experiencing withdrawal. Both are relevant to repeated use of alcohol over time. Individuals may develop alcohol tolerance such that after drinking at sufficiently high levels frequently enough the body begins to adapt to the presence of alcohol. This, in turn, means that homeostasis pressures are operating, and a person will need to either consume greater amounts of alcohol or drink more quickly in order to achieve the expected effects; or, the person will experience diminishing effects from consuming the same amounts over time. Alcohol withdrawal symptoms can range from relatively mild and unpleasant to very serious and potentially fatal; they may begin within hours of when alcohol use ceases to days after the last drink. Mild symptoms of acute alcohol withdrawal might include:
- tremors (e.g., shaky hands)
- headache
- nausea/vomiting
- anxiety
- sleep disorder (insomnia)
- profuse sweating
More serious/severe symptoms of acute alcohol withdrawal might include:
- hallucinations (tactile, auditory, visual)
- seizures
- confusion/disorientation
- rapid heartbeat, high blood pressure, fever
- delirium tremens or DTs (a constellation of symptoms involving severe mental and/or nervous system changes and mostly occur in persons who have engaged in heavy drinking for multiple years).
The mortality rate for acute alcohol withdrawal involving the most severe symptoms ranges from 5-25% (Trevisan et al., 1998)—particularly if the withdrawal is not medically supervised or managed. A person in this state may need to engage in a medically managed detoxification (detox) process in order to be safe. Thus, advising or forcing someone who has severe AUD to abruptly stop drinking is unwise and potentially life-threatening. Quite possibly some deaths attributable to regional natural disasters (e.g., severe hurricanes) may be the result of individuals whose bodies have become dependent on alcohol not having access to alcohol and being forced into acute withdrawal.
Stop and Think
Using the BAC calculator link above (or a similar calculator), enter your own data to determine different scenarios.
- How much, how fast would your own BAC estimate reach or exceed 0.08%?
- What drinking pattern would get you to a point of significant impairment (0.10%-0.12%), severe intoxication (0.25%-0.30%), or risk of coma and loss of consciousness (0.35%-0.40%)?
Alcohol’s cognitive effects. As a CNS depressant, alcohol even at relatively low levels slows the speed of cognitive information processing meaning that it can impair driving and reactions to the point where certain activities become dangerous to self and others. “Alcohol is responsible for approximately half of all trauma deaths and nonfatal injuries in the United States” (https://www.facs.org/~/media/files/quality%20programs/trauma/alcoholinjury.ashx).
For example, alcohol affects most aspects of perception (the first step in information processing). Not only does it have a general effect on the brain, it has a specific effect on the visual and auditory (hearing) areas. Because alcohol blunts lower sound frequencies involved in speech perception, individuals often begin to speak more and more loudly as their level of intoxication rises—this is only partly about disinhibition of cognitively controlled behavior, it is also a matter of changes in how sound is perceived. Next in the information processing sequence, alcohol affects memory processes. Encoding new memories, a critical aspect of learning something new, is impaired by heavy alcohol use. An alcohol-induced “blackout” involves interference with encoding information into memory—the memory is not “lost,” it is simply never created.
With chronic heavy alcohol use, memory retrieval becomes increasingly impaired, as well. A memory may have been adequately stored, but the individual may have difficulty retrieving it at will. Together these two functions being impaired help explain state dependent learning in association with alcohol misuse: when a person learns something new or acquires a memory in an intoxicated state, they may have difficulty retrieving the information later in a sober state. Adolescents and emerging adults in recovery from AUD may find it necessary to repeat large portions of their formal education as the information “learned” during the AUD period may no longer be easily retrieved. Furthermore, heavy alcohol use is associated with the onset and progression of dementia in adulthood.
Not only is alcohol implicated in distortions of perception and memory in information processing, it also can impair decision-making and judgment. A significant literature indicates that drinking alcohol impairs a person’s ability to accurately assess risk or feel appropriate anxiety in potentially risk situations. Thus, a person who has been drinking may make risky choices—diving into shallow water, “hooking up” with an unfamiliar sex partner, ignoring “safe sex” practices, deciding to drive despite knowing it is unwise, spending money they cannot really afford.
Alcohol-related brain damage (ARBD) refers to a group of brain changes, resulting in cognitive and other brain impairments, caused by a person’s prolonged pattern of alcohol misuse. This occurs in about 30% of persons engaged in prolonged heavy drinking (Dalvi, 2012). An example is diagnosed as Wernicke-Korsakoff syndrome. Alcohol-related brain damage is differentiated from the acute effects of intoxication because it is a long-term effect. For example, alcohol-related dementia is diagnosed based on symptoms persisting for more than 2 months after cessation of alcohol use. It may be challenging to differentiate from other forms of dementia (e.g., Alzheimers disease or Lewy body dementia). Some reversal of damage is possible with abstinence (Dalvi, 2012).
Physical health effects. Not only does alcohol have effects on brain and behavior, it also has effects on physical health. First, alcohol also is a known teratogen, meaning that it disrupts fetal development (see the section concerning fetal alcohol exposure). Second, as previously noted, it plays a role in vulnerability to accidental injury. Third, alcohol use/misuse plays a role in intentional self-harm/suicidality through its disinhibition, impulsivity, and impaired judgment effects (Pompili, et al., 2010). Additionally, alcohol misuse may play a role in suicide risk if it interacts with other, pre-existing mental disorders, stress, social withdrawal/marginalization and loss of social bonds (Pompili et al., 2010). Fourth, alcohol has known effects on cardiac (heart) and circulatory system health. For example, as a CNS depressant alcohol can cause a severe slowing of respiration (breathing), to the point where someone could become oxygen deprived. This risk is multiplied when alcohol is combined with other CNS depressant substances.
Evidence concerning the potential positive effects of drinking one standard drink equivalent of wine daily has come under review. The current recommendation is that someone who does not currently drink alcohol should not begin to do so in hopes of improving their health; there are better ways to accomplish this goal (e.g., diet, exercise, medications, and stress-reduction wellness activities).
Alcohol biomarkers. Because of the way that alcohol is metabolized and the role of its metabolites (breakdown byproducts) in health, it is useful to understand a bit about biomarkers sometimes used in assessment. Biomarkers are objective biological indicators of a substance being present, possibly its concentration, the breakdown products (metabolites) of the substance as it is metabolized, and/or the health of the organ systems affected by the substance (e.g., liver, kidneys, gastrointestinal tract).
Breathalyzer test. A breathalyzer is one form of biomarker measure—it provides an estimate of a person’s circulating blood alcohol concentration (BAC) or blood alcohol level (BAL). The breathalyzer can detect the presence of alcohol for about 8 to 12 hours after consumption, but it is not clear on a single test whether a person’s level is still climbing (the first hour or two after drinking) or dropping as the alcohol is metabolized. It is a somewhat controversial tool. First, some brands/manufacturers have better accuracy than others. Second, the breath sample must be properly collected. Third, the device must be properly maintained and regularly calibrated.
Blood, urine, sweat, saliva tests. A blood test is a direct measure of the amount of alcohol circulating in a person’s blood. It is more reliable than a breathalyzer but is also far more invasive. It also relies on two forms of expertise: the blood draw to collect a sample and the laboratory technique to analyze it. Alcohol shows up in a person’s urine, sweat, and saliva, as well. These are less reliable as indicators of amount consumed but can detect the presence of alcohol for hours (not days/weeks) after drinking. Some alcohol metabolites, however, can be detected for a few days.
Clinical tests. Three tests are commonly utilized to determine the effects of regular heavy alcohol consumption on the liver: the GGT, AST, and ALT. Two tests examine effect on blood and plasma: MCV (size of red blood cells/ability to carry oxygen) and CDT (measuring a serum protein carrying iron through the bloodstream). These tests provide information about a person’s health and organ damage; however, disease processes other than AUD may cause their values to be abnormal.
Fetal Alcohol Exposure
“A significant, pervasive, and persistent alcohol-related public health concern is the potential impact of alcohol use and alcohol use disorders among women of child-bearing age and during pregnancy” (Popova, Rehm, & Shield, 2020). Globally, an estimated 10% of women consumed alcohol during pregnancy, and over 25% engaged in binge drinking during pregnancy (Popova, Lange, Probst, Gmel, & Rehm, 2017). Many adverse pregnancy outcomes have been associated with alcohol use: loss of pregnancy or stillbirth, premature delivery, growth retardation and low birth weight, and fetal alcohol spectrum disorder (Popova, Rehm, & Shield, 2020).
Fetal Alcohol Spectrum Disorder (FASD). Prenatal alcohol exposure can cause brain injury resulting in “pervasive, permanent neurodevelopmental differences which impact health, educational, and vocational outcomes” which comprise fetal alcohol spectrum disorder (Loock, Elliott, & Cox, 2020). The risk of FASD increases with binge drinking patterns and/or high quantities of alcohol consumption, and when maternal alcohol absorption is increased (low body weight and poor nutrition/fasting); effects are compounded with concurrent exposure to other substances, including use of tobacco products (Loock, Elliott, & Cox, 2020). In one U.S. study, about 1/3 of pregnant women who reported alcohol use in the past 30 days engaged in binge drinking; among pregnant women who engaged in binge drinking did so an average of 4.5 times during the past 30 days (https://www.cdc.gov/ncbddd/fasd/data.html).
The term “spectrum disorder” is important here because the effects of prenatal alcohol exposure fall extend across a quantitative continuum, as well as varying qualitatively. Some individuals exhibit little or no obvious effects, while others exhibit mild, moderate, or significant differences in physical features or organ system birth defects (malformations of heart, bone, kidney, visual, or hearing systems): alcohol–related birth defects (ARBD). [Note: the abbreviation ARBD is also used to specify alcohol-related brain damage resulting from alcohol misuse later in life.] Others exhibit alcohol-related neurodevelopmental disorders (ARND), referring to complex differences in neurodevelopment that may affect cognition, information processing, language, behavior, attention, executive function, adaptive skills, mood, hyperactivity, and self-regulation as a child matures (https://www.niaaa.nih.gov/sites/default/files/ARNDConferenceConsensusStatementBooklet_Complete.pdf). Fetal alcohol syndrome (FAS) is considered to be the most severe outcome of prenatal alcohol exposure and may be either full or partial in nature (FAS and pFAS). FAS involves morphological differences (e.g., facial features, growth deficiency) and damage to the central nervous system. Because the effects of alcohol exposure affect so many aspects of fetal growth and development, there is no prenatal period when any amount of alcohol exposure is considered safe (https://www.nofas.org/).
How commonly the full range of FASD occurs in the United States remains unknown; estimates “might number as high as 1 to 5 per 100 school children (or 1% to 5% of the population)” (https://www.cdc.gov/ncbddd/fasd/data.html). FAS as the most evident, complicated category is estimated to occur among 3 in 10,000 children aged 7-9 years or up to 90 out of 10,000 children (https://www.cdc.gov/ncbddd/fasd/data.html). What this suggests is that many individuals with whom we engage in daily living or in delivery of human, educational, or health services experience some types of lifelong neurological and/or behavioral effects of prenatal alcohol exposure. Consider also that an infant born with developmental and health challenges related to prenatal alcohol exposure may also enter a social/physical context where parents may be ill-prepared, ill-equipped, or under-responsive to their typical and atypical/exceptional developmental needs.
A group of young adults growing up with FASD conducted a survey of other adults concerning their health as adults prenatally exposed to alcohol (Himmelreich, Lutke, & Hargrove, 2020). They drew several important conclusions from the 541 survey responses:
- Adults with FASD experience vulnerability to a wide range of health conditions, diseases, and disorders, many of which occur at younger ages than in the general population (premature aging).
- FASD over the lifespan is about more than the brain—it is a “whole body” disorder affecting physical and mental health.
- What is “normal” in the general population may not be “normal” for a person with FASD.
- Health and mental health challenges experienced by adults with FASD may be misunderstood, misidentified, misdiagnosed, mistreated, and/or under-served by physical and behavioral health care providers.

